Can MS Make You Sick To Your Stomach?

Note: This is not medical advice. If MS is causing IBS or other gastrointestinal symptoms, talk to your doctor.
Can MS Make You Sick To Your Stomach?
You know that puffy, painful feeling you get after a massive holiday meal? The one where your stomach is stretched to the max and you vow never to eat again; but then your mom brings out the pumpkin pie and you convince yourself a “dessert tummy” is a real thing?
As North Americans, we’re not exactly known for restraint when it comes to food–overindulging is practically part of our value system. Pretty sure it’s treason if you don’t polish off at least two heaping plates at Thanksgiving, and you clearly don’t love your family or baby Jesus Himself if you’re not eating your way through December.
No judgement here. Food is amazing. From raspberry macarons in a Parisian champagne bar to the biggest, best curbside panini in Florence, to a cricket-topped guac in Mexico City, most of my best memories are attached to great meals. Food doesn’t just keep us alive, it gives us a reason to live.

While the occasional overindulgence is normal and definitely worth it (because your dad only makes turkey stuffing twice a year), what’s not a good deal is feeling like a human circle after a kale salad or a saltless mug of bone broth.
Guys. My tummy hurts.
All.The.Time.
It’s baseline for me to completely bypass the satisfied feeling of a belly full of sustenance and go straight to over the belt bloating and stabby pains almost every time I eat. Except I never wear belts and overwhelmingly prefer empire waistlines. The fashionista in me doesn’t believe that “sack” and “dress” should ever be uttered in the same sentence. But when my stomach’s in charge, it refuses to be contained.
My stomach is almost always in charge.

If you have MS like I do, debilitating tummy troubles might be on your list of reasons why this disease is the freaking worst.
My abdominal distress can make it difficult to sleep, exercise, and concentrate. Chronic discomfort makes me say mean things and think meaner thoughts. Socially, I’m either feeling like a party pooper or eating through pain just to be polite.
I’ve been complaining about early satiety, stomach aches, and bloating for years. I’ve seen naturopaths and a gastroenterologist. I’ve experimented with elimination diets. I’ve gone gluten free and tried Whole30. I never ever eat legumes and I rarely eat processed food. Thanks to my Fitbit I can tell you every single thing I’ve consumed since 2017 and there is no rhyme or reason to what causes my digestive system to wig out.
Bowel dysfunction is a widely recognized MS symptom. It’s easy to pin constipation and incontinence on MS. The bowel will not be ignored. But do not underestimate the power of MS to mess with your everything. From dysphagia to diarrhea, MS can cause gastrointestinal symptoms at all stages of the digestive process.
Figuring out what’s wrong with my MSy tummy.
Anyone who lives with anything undiagnosed and under-treated knows that the pursuit of answers can wear you down. I can only use so much energy trying to fix any one of the 247 problems MS causes at any one time. At intervals, I calm down, reassured that I probably don’t have cholera or a tapeworm. Probably. I languish in a state that more or less accepts that like so many MS symptoms, stomach issues are something I have to live with.
But when symptoms inevitably flare again, I re-enter the soul-crushing cycle of searching for solutions. My most recent plea to a new gastroenterologist left me feeling frustrated after I was told my symptoms don’t align with colon cancer, but that he would order a colonoscopy anyway, as well as an anorectal manometry for some reason.
The prep for both these tests is brutal for anyone with a neurogenic bowel. If you’re wondering wtf anorectal manometry is, lucky you. I’m not a doctor, so I can’t claim that an anorectal manometry is more than a bit extra for most of us, but this probe feels like a pretty extreme attempt to prove what we already know about MS.
While I’m tempted to make my gastroenterologist the villain of my gastronintestinal whodunnit, I recognize that this guy was just offering me the tools that are available to him.
One of the most important Q’s empowered patients need to ask is: Is this test/procedure/treatment really necessary?
When I expressed my concerns, my GI shrugged and told me I didn’t have to do the exams if I didn’t want to. When I asked if there was anything else he could offer me, he told me to take Metamucil. (Okay, maybe he is the villain.)
Clearly, I’m on my own here. Feeling like doctors have given up on my gut, I went back to a place that never lets me down: the internet. Here’s what I learned:
MS can cause dyspepsia
The Canadian Society of Intestinal Research validates that MS can cause GI symptoms that go beyond bowel dysfunction and draws a straight line between MS and dyspepsia. Dyspepsia sounds serious and I wonder if that’s what’s ruining my appetite. But when I read further I realize dyspepsia is just a fancy word for indigestion. Indigestion is what your alcoholic grandfather has because all he consumes are Hot Rods and Labatt 50. I refuse to accept that what I’m dealing with can be as simple as indigestion. Do not come at me with a ‘drink-more-water-avoid-carbonated-beverages- chew-your-food-and-eat-fucking-slowly’ solution. I have obviously tried these things.
MS can cause Irritable Bowel Syndrome
Like dyspepsia, IBS feels like a vague non-diagnosis; the thing they call the thing that they don’t know what the thing is. IBS feels like it goes with the word “just”. As in, “relax, it’s not cancer, it’s just IBS.” And, again, I say How dare you? I am suffering here. Irritable is what I become when I order brunch and my eggs arrive over-poached. Talk to me when you change the name to Homicidal Bowel Syndrome and I might reconsider HBS as a valid possibility.
MS is a risk factor for Gastroparesis
Gastroparesis is a condition that impacts the stomach’s ability to move food to the small intestine in a timely manner, and the more I learn about it, the more I start to believe that this is what’s happening with me. My arms, legs, and even my eyes are slow and uncoordinated. Not to mention my bowel and bladder. I also have a touch of dysphagia, which throws my swallowing out of whack. When everything around and connected to my stomach struggles to work together, it makes sense to me that my stomach would also be phoning it in. And nobody’s answering.

My physiatrist agreed to send me for a gastric emptying study. Sidebar: I will post about physiatry later; and no, I’m not mis-spelling psychiatry. If you can get yourself a physiatrist do so. Physiatrists are the best people alive.
Preparing for a gastric emptying study
Unlike prepping for a colonoscopy or an anorectal manometry (I swear that’s the last time I will type that vile word), the prep for a gastric emptying study was not the worst. The hardest part was the need to skip my bowel meds (magnesium hydroxide, and psyllium, aka Metafuckingmucil) for 48 hours beforehand. And sure, this sounds like NBD, but if a butterfly flaps its omnipotent wings in Timbuktu, the delicate balance of my precious bowel routine will be thrown completely off course. It will take me at least a week to get back on track.
The day of the test I arrived at the hospital at 8am to eat a radioactive cheese sandwich. Then, at regular intervals, I slid into a scanner so a tech could take pics to see how far my breakfast had traveled.
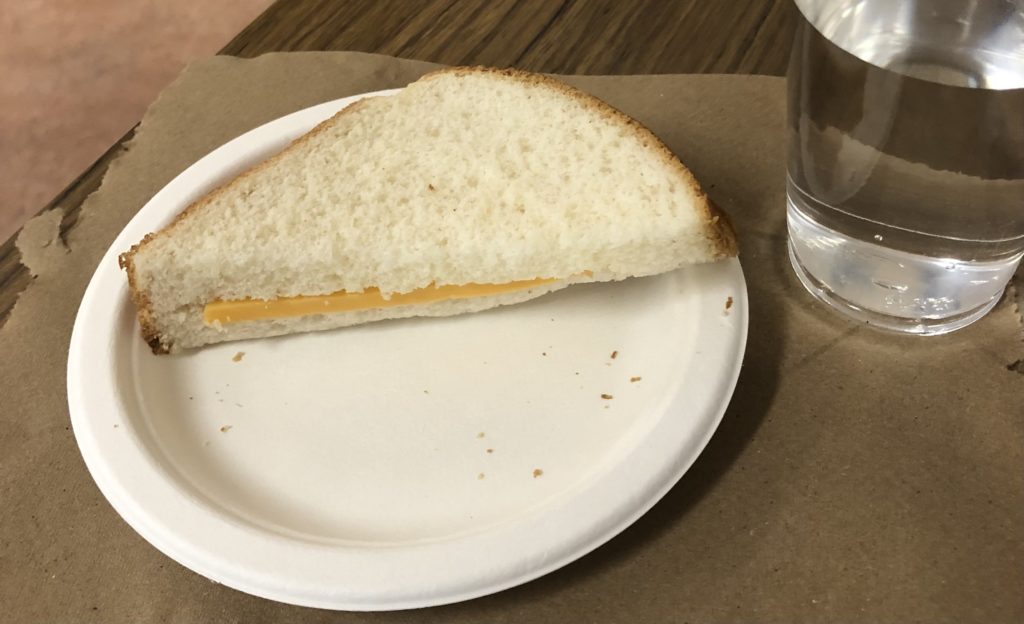
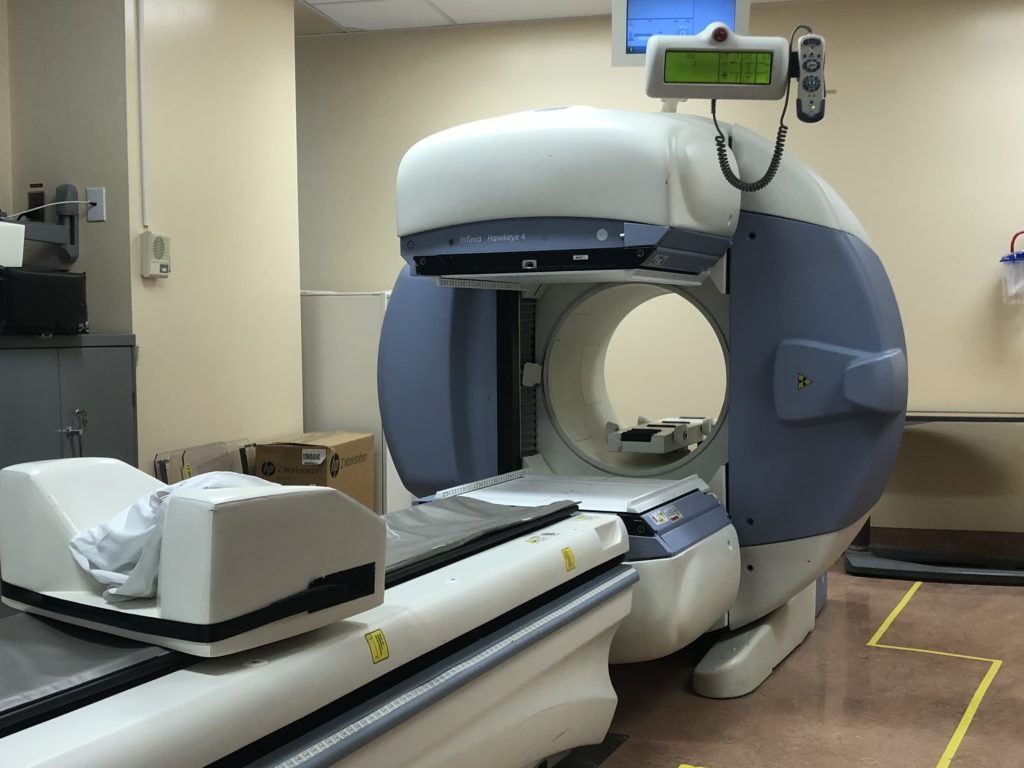
I was told I could leave after my 10:30 photoshoot if the sammy had traveled far enough. When I wasn’t released until 12.30–the maximum length of the test, no matter how far that sandwich had journeyed, I felt vindicated–certain that my advanced patient-knowledge and self-advocacy had led me to the solution to my problem. No matter that the tech, who for legal and bureaucratic reasons was not allowed to give me any actual intel, cautioned me not to interpret my own results.
As I waited for my test results I started looking into gastroparesis diets. Fruits and vegetables are the foundation of my current diet but can be problematic for GP patients. Would my gastronomic future be limited to boiled chicken and baked potatoes? What would Terry say? Of course, the good news here is bagels, because unless you have celiac disease, the GP diet gives two thumbs up to bread. Still, it felt a bit sketchy because no diet ever recommends bread.

I got my test results by email later the same day. You guys already know what happened. In the frustrating double-edged gut-wrenching reality of the chronically ill, my test results were normal. Of course they were.
I would eat crow if I thought it would help.
MS and IBS
I can’t help but wonder if the test had been done later in the day, there might have been a different result. My legs perform dramatically differently at 8 am than they do at quitting time, so why wouldn’t my stomach? Nevertheless, I’m willing to reconsider that IBS is more complex than I give it credit for and that maybe that’s exactly what’s going on. The most compelling evidence of the potential of “just IBS” is that despite feeling like my own death is imminent, I’ve been suffering for literal years and I’m not actually dead.
I went back to the Canadian gastro site looking for IBS life hacks and found this gem:
“Over time, with understanding and faithful adherence to an individualized treatment plan, many patients with irritable bowel syndrome can look forward to a notable improvement in their condition. In fact, statistics show that approximately 10% of IBS patients get better each year.”
Excuse me? 10%? TEN PERCENT???
Back to the naturopath I go for more tests and guidance. Spending more of my money and time and mental and emotional real estate just trying to feel okay.
In the meantime, if anyone knows where I can get a fecal transplant (is that a thing yet?), lemme know. I will try anything.

Follow Tripping On Air on Facebook and Instagram

 Back to
Back to
Gas. A perfectly normal day turns uncomfortable when I feel pressure down there. I try to let it out in short bursts but it explodes out of me. I was waiting to cross the road and I noisily let it out. Three guys who happened to walk behind me at that moment, complimented me.
Gross, Joe. Super gross.
Yes to all of this. Severe cramping and gas, which keep me up at night. I have a prior diagnosis of UC, but that hasn’t reared its ugly head in 12 years. Right now, after a plain bowl of pasta, Im having heartburn up to my eyeballs, through my back and under my arms, despite the max. dose of PPI and added Tagamet before dinner. I’m on my 8th gastro and I like her. Just had my 6th colonoscopy and 8th endoscopy with multiple biopsies, enzyme test and tests for 22 pathogens. Aside from a small hiatal hernia, which the GI said can’t account for my constant agony and lately, unrelenting diarrhea, I have the GI tract of a healthy teenager. I do have more food allergies than I can count (all salicylates and a severe histamine intolerance (BTW bone broth is really high in histamines) and can’t eat any fruits or vegetables or fiber without almost calling 911. So, I’m staring at the SIBO test on my dresser which I suspect I have a severe case of and Dr. Williams puts his money on Mast Cell Disorder, too. FMT is great for UC, but might not be the best idea for SIBO, because the bacteria in the colon can travel up into the SI and make the situation worse. I don’t know about Canada, but FMT is really only approved for C-Diff here. I hope you get some relief…We all need a break from this. At least we should be able to enjoy food! Hope you get a diagnosis and treatment that works.
So interesting. Thanks for sharing. I had no idea bone broth was high in histamines.
I have mast cell activation (developed after Lemtrada) and I suspected it after my most recent week of abdominal pain (I’d been playing fast and loose with my antihistamine. )
Three cheers for Dr Williams.
Keep me posted.
https://www.nytimes.com/2021/08/02/well/live/irritable-bowel-syndrome-treatments-causes.html. Read this a few weeks ago…
Another great essay, Audra! You are a fantastic writer, and your comedy is on-point! XOXO
Andy
Thanks for reading, Andy.
Ditto !! I love, love , love reading and the comedy is icing on the cake! Thank you!!
Been there well before I new I had MS. I’ve given up on tests because the results never seem to tell me anything actionable, although I did take antibiotics for SIBO one time that may have helped a little. The best solution I ever found was just eating as little as possible ?
What a revelation! I had no idea that my gastrointestinal problems (uncontrollable farting and bowel movements) were so closely tied to MS. But as you say, you can only work on so many MS problems at a time and my physiatrist did recommend Metamucil so i have been taking it faithfully for years (i love him anyway btw). But the IBS always gets pushed to the side during appointments for more important issues like walking and cognitive function(or lack there of). Anyhoo, it’s nice to hear this isn’t all in my head, although i wouldn’t wish this on anyone! Thanks Ardra,you’re pieces are always spot on and I’d laugh harder but i might poop or pee my pants! Lol
About ten years ago I went through a period in time when I thought I had IBS. It was awful, my bowel had a mind of its own and wouldn’t take no for an answer. It was socially horrifying and I was continually under great amounts of stress when I stepped outside my house.
I went to a naturopath and she suggested trying a colon cleanse. I dragged my feet but eventually gave in out of desperation. I’m not sure what happened but my IBS symptoms went away. I’m not sure if it was just a coincidence but the timing was spot-on and all my IBS symptoms disappeared.
This procedure has mixed reviews throughout the internet but I’m personally glad I tried it. All the best with these gastronomic issues Ardra. ?
My physiatrist (at a MS clinic in Toronto, wouldn’t refer me to a gastroenterologist, told me to go through my family doc but he is not familiar with specialists who deal with patients with neurological disorders and patients on wheelchairs. Do you know if your gastroenterologist is familiar with neurological cases? If yes, do you mind telling me who you see? I’m in the GTA but most of my specialist appointments are in Toronto.
Please know I’m not trying to preach here because everyone’s digestive system is different. Even pre-MS I always had gut issues and constipation was the norm. By trial and error I discovered dairy was not my friend. One thing led to another and before I knew it, I had joined the ranks of the whole food plant based tribe. Nothing processed, obviously no animal products consumed, no oil and moderate intake of salt and sugar (I know, is this a life?). It turns out the goal to calm my irritable gut outweighs my need for “fun” food. I adjusted my taste buds to like real food (I’m not kidding) and my regular morning BM’s are nothing but stellar. Sometimes there’s a repeat performance later in the day. But one thing was worse and that was the gas and bloating. I was eating high fibre including legumes so you know how it goes – pop, pop, fizz, fizz down there. Not fun and I almost abandoned this wonderful way of eating I discovered. So behold, I found a plant based gastro and eagerly sought his guidance. Turns out like all the rest he pulled out the invasive tests. Tubes down this away and up that away. I said no thanks, I was pretty certain I didn’t have celiac disease since I don’t eat gluten. I’m happy to say, without any invasive tests or the opinions of any health care provider most of whom have limited nutritional education, I solved my gas and bloating (so proud and amazed to this day). Out of desperation I yet again embraced Beano (after years of half hearted trials) and another high performance enzyme supplement with an impressive list of ingredients. I took them together before/during each meal. I’m beyond happy to report that they worked their magic down there and I’m about 90% free of the noise and discomfort of a bowel working overtime. Obviously this is not everyone’s problem and enzymes are not going to be everyone’s salvation. I wanted to share this not to say “you should too” but maybe when something this life changing happens you have to shout it from the roof tops. Cause gut issues ain’t fun. P.S. the enzyme I tried (other than Beano) is Enzymedica Gold. I chose it because it has a ton of the little enzyme guys.
Thanks Ardra for bringing these things to the forefront. It’s such a big annoying part of MS.
Omg I am sooo sorry about what you are going through. I realize doctors only have a certain bag of tricks, but it seems like they should want to be better. Your sharp pains with eating remind me of something that was happening to me after I had gone for a bone density test. A stranger on the internet responded to a post I made about it and mentioned to at it might be calcium supplements. Duh- I hadn’t bothered to think about what I’d been doing differently. After the bone scan they told me to start taking calcium. Apparently it’s like sandpapering your innards for some people. I’ve learned that certain magnesium pills can do this too, but to a lesser degree. I dropped those pills and my issue resolved. I know it’s so frustrating to hear everyone’s suggestions, and that may not be what’s going on with you at all, so I’m sorry if I’m just adding to the noise, but for what it’s worth, I hope it helps, and if not, I really hope you find answers and actionable advice?.
My pain is in my ass. You know, literally. Chronic constipation. It’s relentless. Lots of things work, but often too well. And nothing works consistently.
***head bangs on wall***
Leaving the house for more than an hour is like playing Russian roulette.
As the others have said, thank you. I’ve been having a “full” sensation for a couple of months at least lately. My GP could find nothing wrong and as was noted by someone else, the visit to my specialist did not concern itself with my gut. But your descriptions hit nails on the head and I thank yo for this.
I immensely enjoy your perspective, your wit, and your writing style. Have any of your doctors ever brought up pudundal neuralgia, which can impact bowels, pelvis floor/digestion, and sexual sensation? I’ve had MS for over 30 years, but only learned about this condition recently. Might be worth checking out.
Suz Y.
Well, all of us non muggle MS folk know Dante missed one circle – the tenth one reserved for MS. But sometimes, just sometimes, a small warm beam of light makes it down there. As in you end up getting an answer with an actual solution to one of the zillion things your body is refusing to do. (Or in the case of stomach/bowels doing a bit too well) Something that turns out to be simple. (Simple and MS don’t belong in the same sentence.) After a myriad of tests (your nuclear cheese sandwich should have been a nuclear donut to match the MRI machine Ardra) I came to find out that Fecal Impact (not the movie Fatal Impact) was causing pretty much all my stomach/intestinal woes. And the solution? ….drumroll please….senna. That’s right, the everyday non prescription stuff you get at any drug store. I won the poop lottery. I was so excited I almost kicked my non functional leg and foot in the air from my chair. Yup, I will now be extolling the virtues of senna. Metamucil sits there like a log – it’s not a mover and a shaker like senna. Yeah, yeah – we all get the drink more water and do as much physical activity as you can deal. Whatever. Bite me. All I know is I was thrilled beyond belief to not be pronounced MS and IBS for better or worse. So….WWTD? (What would Terry do?) Probably invent a new diet built around…senna.
I’m pretty excited, and wish all my fellow non muggles the best of luck on their bowel journey. Tom Petty and myself got lucky babe.
Interesting read! And here I thought my IBS predated my MS diagnosis but now I think maybe that was the start of my MS!!
Obviously not a doctor, but my gastro prescribed me Dicetel and it has been a game changer. Is an IBS med that gives me a chance.
Thanks for the tip. I will look this up.
IBS is debilitating. I have IBS-C and that means basically no pooping for days and days without meds (I take Trulance). The constipation begets bloating, pain, mild nausea and reflux. The meds cause 4-5 very…shall we say violent, bouts of diarrhea that lasts about half a day. This means readjusting your schedule, sometimes skipping days, caution when traveling, etc. I have all the symptoms you describe. Diet won’t fix it. When I don’t take the meds, I also have very slow moving bowels. There is also IBS-D which is diarrhea forever basically. Maybe try the meds just to see if they help?
Thanks for sharing your experience, Vicky. I’m always nervous to mess with bowel meds, preferring the enemy I know. But sometimes it helps to find new approaches.
Sorry I’m late to the game here, but I just found your blog yesterday. I have to say as a fellow Canadian, I’m impressed that you have access to both a gastroenterologist and a physiatrist! I’ve had IBS since I was two weeks old and have never been referred to either. Anyway, thank you for sharing your story. Misery loves company I guess, because it feels good to know you’re not alone, right?
Not sure the gastro is helping me all that much, but definitely recommend getting on a list to see a physiatrist if possible.